Endometriosis
-
Endometriosis
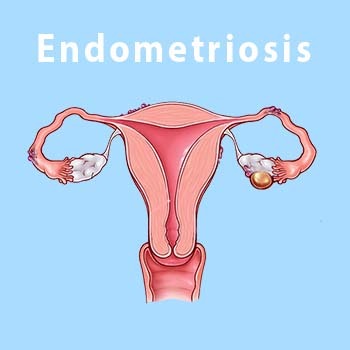
More than a million women across the world contracts Endometriosis in their lifetime. Exact nature of endometriosis hasn’t been determined, although the symptoms are invisible, but the condition is associated with an acute pain in the pelvic region. Before comprehending endometriosis, one must know what endometrium means, it is the mucus lining of the womb or uterus. The endometrium would get rekindled throughout the menstrual cycle. When the woman gets pregnant, the endometrium would get thickened and is supplied with vasculature, however if the woman does not get pregnant the endometrium tends to shed, that is the reason for menstrual bleeding.
Endometrium is the inner lining of the uterus which sheds during periods and grows back. Endometriosis is an often-painful condition in which tissue that is similar to the inner lining of the uterus grows outside the uterus. It often affects the ovaries, fallopian tubes and the tissue lining the pelvis. Endometriosis growths may be found beyond the area where pelvic organs are located.
Endometriosis tissue acts as the lining inside the uterus would — it thickens, breaks down and bleeds with each menstrual cycle. But it grows in places where it doesn't belong, and it doesn't leave the body. When endometriosis involves the ovaries, cysts called endometriomas may form. Surrounding tissue can become irritated and form scar tissue. Bands of fibrous tissue called adhesions also may form. These can cause pelvic tissues and organs to stick to each other.
Endometriosis can cause pain, during menstrual periods, fertility problems etc. But treatments can help you take charge of the condition and its complications.
Endometriosis impacts commonly people between the age of 25 and 40years. It can also happen to younger people during teenage.
-
Symptoms
The main symptom of endometriosis is pelvic pain during menstrual periods. Although many people have cramping during their periods, those with endometriosis often describe menstrual pain that's far worse than usual. The pain also may become worse over time.
Common symptoms of endometriosis include:
Painful periods. Pelvic pain and cramping may start before a menstrual period and last for days into it. You also may have lower back and stomach pain.
Pain with sex. Pain during or after sex is common with endometriosis.
Pain with bowel movements or urination. You're most likely to have these symptoms before or during a menstrual period.
Excessive bleeding. Sometimes, you may have heavy menstrual periods or bleeding between periods.
Infertility. For some people, endometriosis is first found during tests for infertility treatment.
Other symptoms. You may have fatigue, diarrhea, constipation, bloating or nausea. These symptoms are more common before or during menstrual periods.
The seriousness of your pain may not be a sign of the number or extent of endometriosis growths in your body. You could have a small amount of tissue with bad pain. Or you could have lots of endometriosis tissue with little or no pain.
Still, some people with endometriosis have no symptoms. Often, they find out they have the condition when they can't get pregnant or after they get surgery for another reason.
A few places you can develop endometriosis include :
- Outside and hack of your uterus
- Fallopian tubes
- Ovaries
- Vagina
- Peritoneum( the lining of your abdomen and pelvis)
- Bladder and ureters
- Intestines, rectum
- Diaphragm
-
Causes
The exact cause of endometriosis isn't clear. But some possible causes include:
Retrograde menstruation. This is when menstrual blood flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. The blood contains endometrial cells from the inner lining of the uterus. These cells may stick to the pelvic walls and surfaces of pelvic organs. There, they might grow and continue to thicken and bleed over the course of each menstrual cycle.
Transformed peritoneal cells. Experts suggest that hormones or immune factors might help transform cells that line the inner side of the abdomen, called peritoneal cells, into cells that are like those that line the inside of the uterus.
Embryonic cell changes. Hormones such as estrogen may transform embryonic cells — cells in the earliest stages of development — into endometrial-like cell growths during puberty.
Surgical scar complication. Endometrial cells may attach to scar tissue from a cut made during surgery to the stomach area, such as a C-section.
Endometrial cell transport. The blood vessels or tissue fluid system may move endometrial cells to other parts of the body.
Immune system condition. A problem with the immune system may make the body unable to recognize and destroy endometriosis tissue.
Factors that raise the risk of endometriosis include:
- Nulligravida (Never given birth)
- Starting your period at an early age.
- Going through menopause at an older age.
- Short menstrual cycles
- Heavy menstrual periods that last longer than seven days.
- Having higher levels of estrogen in your body or a greater lifetime exposure to estrogen.
- Low body mass index.
- One or more relatives with endometriosis, such as a mother, aunt or sister.
Any health condition that prevents blood from flowing out of the body during menstrual periods also can be an endometriosis risk factor. So can conditions of the reproductive tract such as vaginal septum, cervical atresia etc..
-
Infertility
The main complication of endometriosis is trouble getting pregnant, also called infertility. Up to 3% of ladies with endometriosis have a hard time conceiving.
For pregnancy to happen, an egg must be released from an ovary. Then the egg has to travel through the fallopian tube and become fertilized by a sperm cell. The fertilized egg then needs to attach itself to the wall of the uterus to start developing. Endometriosis may block the tube and keep the egg and sperm from uniting. But the condition also seems to affect fertility in less-direct ways. For instance, it may damage the sperm or egg.
Even so, many with mild to moderate endometriosis can still conceive and carry a pregnancy to term. Doctors will advise those with endometriosis not to delay having children. That's because the condition may become worse with time. It is a progressive disease.
-
Cancer
Some studies suggest that endometriosis raises the risk of ovarian cancer. But the overall lifetime risk of ovarian cancer is low to begin with. And it stays fairly low in people with endometriosis. Although rare, another type of cancer called endometriosis-associated adenocarcinoma can happen later in life in those who've had endometriosis.
- Pelvic exam. Your health care professional feels areas in your pelvis with one or two gloved fingers to check for any unusual changes. These changes can include cysts on the reproductive organs, painful spots, irregular growths called nodules and scars behind the uterus. Often, small areas of endometriosis can't be felt unless a cyst has formed.
- Ultrasound. It can find cysts linked with the condition called endometriomas.
- Magnetic resonance imaging (MRI). MRI helps with surgical planning. It gives your surgeon detailed information about the location and size of endometriosis growths.
-
Treatment
Treatment for endometriosis often involves medicine or surgery. The approach you and your health care team choose will depend on how serious your symptoms are and whether you hope to become pregnant.
Typically, medicine is recommended first. If it doesn't help enough, surgery becomes an option.
-
Pain medicines
Your doctor may recommend pain relievers that you can buy without a prescription. These medicines include the nonsteroidal anti-inflammatory drugs NSAIDs. They can help ease painful menstrual cramps.
-
Hormone therapy
Sometimes, hormone medicine help ease or get rid of endometriosis pain. The rise and fall of hormones during the menstrual cycle causes endometriosis tissue to thicken, break down and bleed. Lab-made versions of hormones may slow the growth of this tissue and prevent new tissue from forming.
Hormone therapy isn't a permanent fix for endometriosis. The symptoms could come back after you stop treatment.
Therapies used to treat endometriosis include:
- Hormonal contraceptives. Birth control pills help control the hormones that stimulate endometriosis. Many have lighter and shorter menstrual flow when they use hormonal birth control. Using hormonal contraceptives may ease or get rid of pain in some cases. The chances of relief seem to go up if you use birth control pills for a year or more with no breaks.
- Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists. These medicines block the menstrual cycle and lower estrogen levels. These medicines create an artificial menopause those include hot flashes, vaginal dryness and bone loss. Menstrual periods and the ability to get pregnant return when you stop taking the medicine.
- Progestin therapy. Progestin is a lab-made version of a hormone that plays a role in the menstrual cycle and pregnancy. A variety of progestin treatments can stop menstrual periods and the growth of endometriosis tissue, which may relieve symptoms. Progestin therapies include a tiny device placed in the uterus that releases levonorgestrel (Mirena), or a progestin-only birth control pill.
- Aromatase inhibitors. These are a class of medicines that lower the amount of estrogen in the body.
-
Conservative surgery
Conservative surgery removes endometriosis tissue. It aims to preserve the uterus and the ovaries. If you have endometriosis and you're trying to become pregnant, this type of surgery may boost your chances of success. It also may help if the condition causes you terrible pain — but endometriosis and pain may come back over time after surgery.
Your surgeon may do this procedure with small cuts, also called robotic surgery. Less often, surgery that involves a larger cut in the abdomen is needed to remove thick bands of scar tissue. But even in severe cases of endometriosis, most can be treated with the robotic method.
-
Fertility treatment
Endometriosis can lead to trouble getting pregnant. If you have a hard time conceiving, your health care team may recommend fertility treatment. You might be referred to a doctor who treats infertility. Fertility treatment can include medicine that helps ovaries make more eggs. It also can include a series of procedures that mix eggs and sperm outside the body, called in vitro fertilization. The treatment that's right for you depends on your personal situation.
-
Hysterectomy with removal of the ovaries
Hysterectomy is surgery to remove the uterus. Taking out the uterus and ovaries was once thought to be the most effective treatment for endometriosis. Today, some experts consider it to be a last resort to ease pain when other treatments haven't worked. Other experts instead recommend surgery that focuses on the careful and thorough removal of all endometriosis tissue and nodules.
Having the ovaries removed, also called oophorectomy, causes early menopause. The lack of hormones made by the ovaries may improve endometriosis pain for some. But for others, endometriosis that remains after surgery continues to cause symptoms.
-
Lifestyle and home remedies
It may take time to find a treatment that works. Until then, you can try some things at home to ease your pain.
- Warm baths and a heating pad can help relax pelvic muscles. This lessens cramping and pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can help ease painful menstrual cramps.
Complications